What is Digital Mammography?
Digital mammography directs a low dose X-ray through the breast, exposing patients to very little radiation while finding potentially invasive cancers.
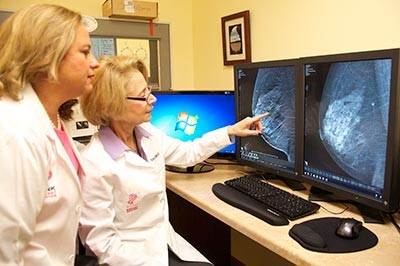
Specially designed digital detectors produce a detailed image that is displayed on a high-resolution computer monitor. Most women begin annual mammogram screenings by age 40. If a screening identifies an area of concern, the radiologist may request a diagnostic digital mammogram. The radiologist will then review the area of concern in more detail and make an appropriate recommendation to you. If we have your prior images available, you should receive your results within 24 to 48 hours. Insurance companies cover Screening Digital Mammograms 100% with no out-of-pocket cost to you.
How Does It Detect Breast Cancer?
Breast cancer, the uncontrolled growth of cells in the breast, is the most common type of cancer among women, excluding skin cancer. Each year in the United States, nearly 230,000 (source NCI) women and 2300 men are diagnosed with breast cancer. A woman has a 1 in 8 chance of being diagnosed with breast cancer at some time during her life. If your mother, sister, or daughter had breast cancer, your chances of getting it are greater. However, four out of five women who get breast cancer have no history of it in their family. The most effective way to detect breast cancer in its early stages is a program of monthly breast self-examination, annual examination by your doctor, and annual digital mammography. Annual digital mammograms are the best tests doctors have to find breast cancer early, sometimes up to three years before it can be felt.
How Is a Digital Mammogram Done?
You will stand in front of a special X-ray machine. A technologist will place your breast on a clear plastic plate. Another plate will firmly press your breast from above. The plates will flatten the breast, holding it still while the X-ray is being taken. You will feel some pressure, but this should not be painful. The steps are repeated at a different angle for a side view of the breast. The other breast will be X-rayed in the same way. Compression reduces the need for radiation and the tissue is better visualized.
PINK Breast Center has seen PINK digital mammography expose patients to less radiation than they were exposed to in prior years. Siemens’ research has confirmed exams done on their Inspiration and Revelation systems use significantly less compression to achieve excellent image quality, with a 30%-50% reduction in radiation exposure compared to traditional digital mammogram systems. A PINK Breast Center Digital Mammogram is a faster, more comfortable digital mammogram.

You will then wait while the technologist checks the X-rays to make sure the images are acceptable and do not need to be retaken. Keep in mind, the technologist cannot tell you the results of your digital mammogram. Each woman’s digital mammogram may look a little different because all breasts are a little different.
What Does Having a Digital Mammogram Feel Like?
Having a digital mammogram is uncomfortable for most women, but you should not find it painful. PINK Breast Center uses Siemens Inspiration and Revelation technology that requires up to half the compression of other systems. It has the lowest compression system we are aware of. A digital mammogram takes only a few moments and any discomfort is over quickly. What you feel depends on the skill of the technologist, the size of your breasts, whether you may have an infection, and how much they need to be pressed. Your breasts may be more sensitive if you are about to get or if you have your period. For comfort, it is best to schedule your digital mammogram 7-10 days after the onset of your last menstrual cycle. A doctor with special training, called a radiologist, will read the digital mammogram. The doctor will look at the X-ray for early signs of breast cancer or other problems.
What Do Digital Mammograms Show?
Digital Mammograms can’t prove an abnormal area is cancer, but they help healthcare providers decide whether more testing is needed. The two main types of breast changes found with a Digital Mammogram are calcifications and masses.
Calcifications are tiny mineral deposits within the breast tissue. They look like small white spots on the pictures. They may or may not be caused by cancer. A tumor may or may not have calcifications, and is another important change seen on digital mammograms. Masses can be many things, including cysts (fluid-filled sacs) and non-cancerous solid tumors, but they could also be cancer. Any mass that’s not clearly a simple fluid-filled cyst usually needs to be biopsied. (A biopsy is taking out a small piece of tissue to see if cancer cells are in it.)
Having your prior digital mammograms available for the radiologist is very important. They can help to show if a mass or calcification has changed over time, which could affect whether a biopsy is needed.
Are Digital Mammograms Safe?
The benefits of digital mammography outweigh any possible harm from the radiation exposure. Modern machines use low radiation doses to get high quality breast images. On average, the total dose for a typical Digital Mammogram with two views of each breast is about 0.4 mSv. (An mSv is a measure of radiation dose.) On the PINK Breast Center Siemens System, our radiation dose is even lower! We work to ensure each and every one or our patients have the absolutely lowest possible radiation dose with the best images.
To put that dose into perspective, people in the US are normally exposed to an average of about 3 mSv of radiation each year just from their natural surroundings. (This is called background radiation.) The dose of radiation used for a screening digital mammogram of both breasts is about the same amount of radiation a woman would get from her natural surroundings over about seven weeks.
If there’s any chance you might be pregnant, let your physician and technologist know. Although the risk to the fetus is likely very small, screening digital mammograms aren’t routinely done in pregnant women.
