What is venous insufficiency?
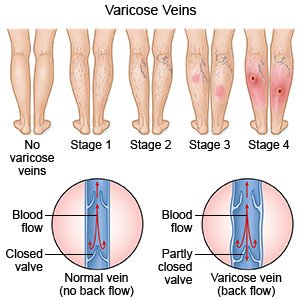
Venous insufficiency is a condition that prevents blood from flowing out of your legs and back to your heart. Veins contain valves that help blood flow in one direction. Venous insufficiency means the valves do not close correctly or fully. Blood flows back and pools in your leg. This can cause problems such as varicose veins. Venous insufficiency may also be called chronic venous insufficiency or venous stasis.
What increases my risk for venous insufficiency?
- A leg injury or blood clot
- Being a woman
- Pregnancy
- Older age
- A family history of varicose veins
- Smoking cigarettes
- Obesity, or not getting enough exercise
What are the signs and symptoms of venous insufficiency?
- Visible veins on your legs that may be small and red or large, thick, and blue
- Swelling in your ankles or calves
- Changes in skin color, such as dark or purple skin
- An ulcer (open sore) on your leg
- Leg pain that is worse when you are menstruating (women) or when you stand and better when you elevate your legs
- Burning or itching
- Cramps that happen at night
- Thick, hard skin on your legs and ankles
- Feeling of heaviness in your legs
-
How is venous insufficiency diagnosed?
- Venous duplex imaging is a procedure used to examine the blood flow through veins. A gel will be applied to your legs. Your healthcare provider will slide a small transducer across the veins. The transducer is a microphone that helps your healthcare provider hear blood moving through the vein.
- Contrast venography is a procedure used to show the veins on x-ray pictures. A catheter is guided into the vein. Contrast liquid is injected into the catheter to help the veins show up better in the photos. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- Plethysmography is a procedure that may be used to find changes in blood pressure through your veins. You will wear a blood pressure cuff on your leg. Changes in pressure and the amount of blood that can circulate through your leg veins are measured while you stand, sit, and lift your leg.
How is venous insufficiency treated?
- Medicine may be given to improve blood flow. The medicines may thin your blood or reduce swelling to help blood flow. You may also need therapy to treat a bacterial infection.
- Ablation is a procedure used to close varicose veins. A catheter is guided until it is near the vein. A device is then guided to the area. The device may produce energy through radiofrequency or a laser. The energy creates heat that closes the blood vessels.
- Sclerotherapy is a procedure used to fade visible veins. Your healthcare provider will inject a liquid into a spider or varicose vein. The liquid irritates the vein, which swells and sticks together. Your body will then absorb the vein.
- Surgery may be needed if other treatments do not work. Surgery may be used to repair a leg vein valve or to clip or tie off a vein so blood cannot flow through it. You may need to have a vein removed during surgery called stripping. Surgery may be used to bypass (go around) the damaged vein. Blood will flow through a vein transplanted from another part of your body.
What can I do to manage my symptoms?
- Wear pressure stockings as directed. Pressure stockings help keep blood from pooling in your leg veins. Your healthcare provider can prescribe stockings that are right for you. Do not buy over-the-counter pressure stockings unless your healthcare provider says it is okay. They may not fit correctly or have elastic that cuts off your circulation. Ask your healthcare provider when to start wearing pressure stockings and how long to wear them daily.
- Do not sit or stand for long periods. If you must sit long, flex and extend your legs, feet, and ankles. Do this about ten times every 30 minutes to help keep blood flowing. If you must stand for a long time, take breaks and sit with your legs elevated.
- Elevate your legs. To reduce swelling, elevate your legs above the level of your heart. Your healthcare provider may recommend keeping your legs elevated for 30 minutes. You may need to do this 3 to 4 times daily, or more if your healthcare provider recommends it.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Reach or maintain a healthy weight. Extra weight can make venous insufficiency worse. Ask your healthcare provider what a healthy weight is for you. He or she can help you create a weight loss plan if you need to lose weight.
-
- Exercise as directed. Walking can help increase blood flow in your calves. Ask your healthcare provider how much exercise you need each day and which exercises are best for you.
- Care for your skin. Keep your skin clean. Do not use any soaps or lotions that may dry your skin. For example, do not use products that contain fragrance or alcohol. Your healthcare provider may recommend a wet-to-dry bandage if you have a skin ulcer. To do this, apply a wet bandage to your wound and allow it to dry. This will help remove drainage from your wound each time you change the bandage. Your healthcare provider will tell you how often to change your bandage and which kind of bandage to use. Check your wound for signs of infection, such as swelling or pus.
- Go to physical therapy (PT) as directed. A physical therapist can help you increase your leg movement and range of motion.
When should I seek immediate care?
- You have a wound that does not heal or is infected.
- You have an injury that has broken your skin and caused your varicose veins to bleed.
- Your leg is swollen and stiff.
- You have pain in your leg that does not go away or gets worse.
- Your legs or feet are turning blue or black.
- Your leg feels warm, tender, and painful. It may look swollen and red.
When should I call my doctor?
- You have a fever.
- You have varicose veins, and they are painful.
- You have new or worsening leg pain, swelling, or redness.
- You have new or worsening ulcers or other sores on your leg.
- You have questions or concerns about your condition or care.
ImageCare can diagnose and treat Venous Insufficiency. To schedule a consultation with one of our Interventional Vein specialists, please call 973-810-8100